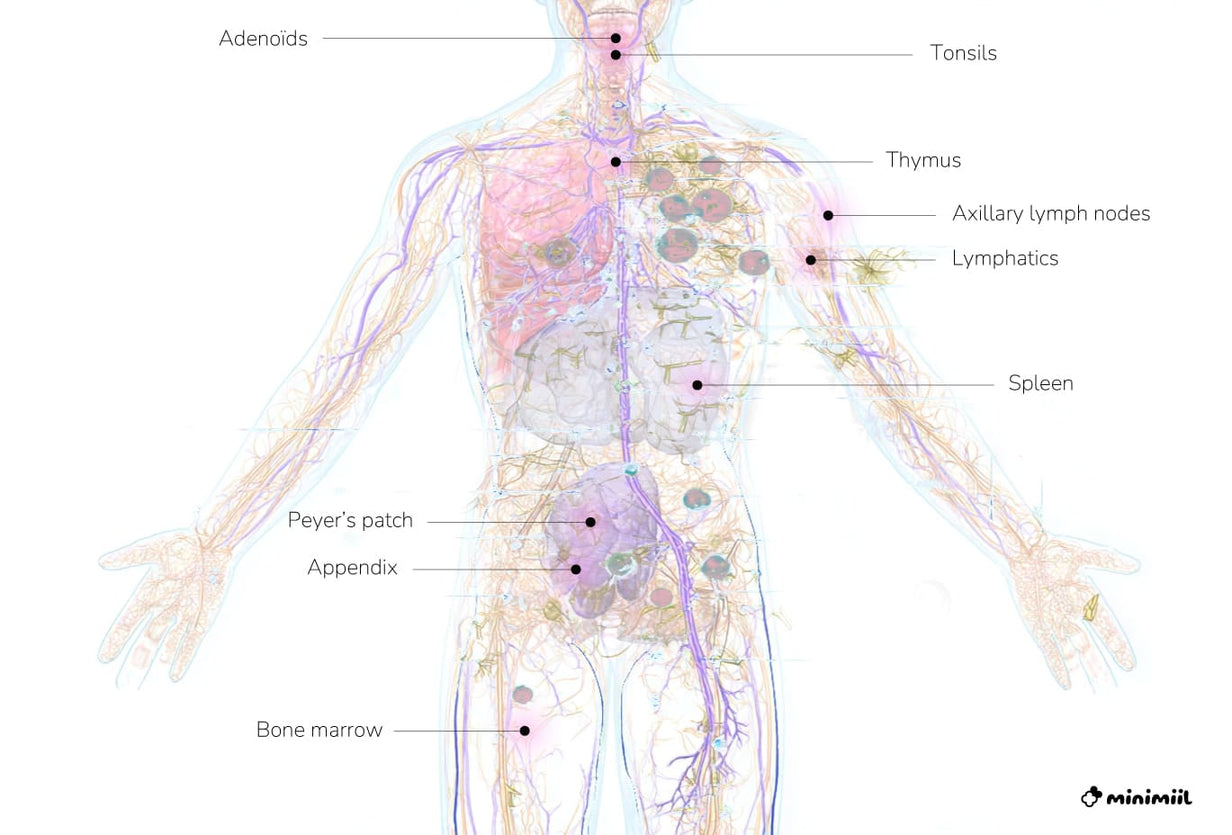
What the Immune System Does
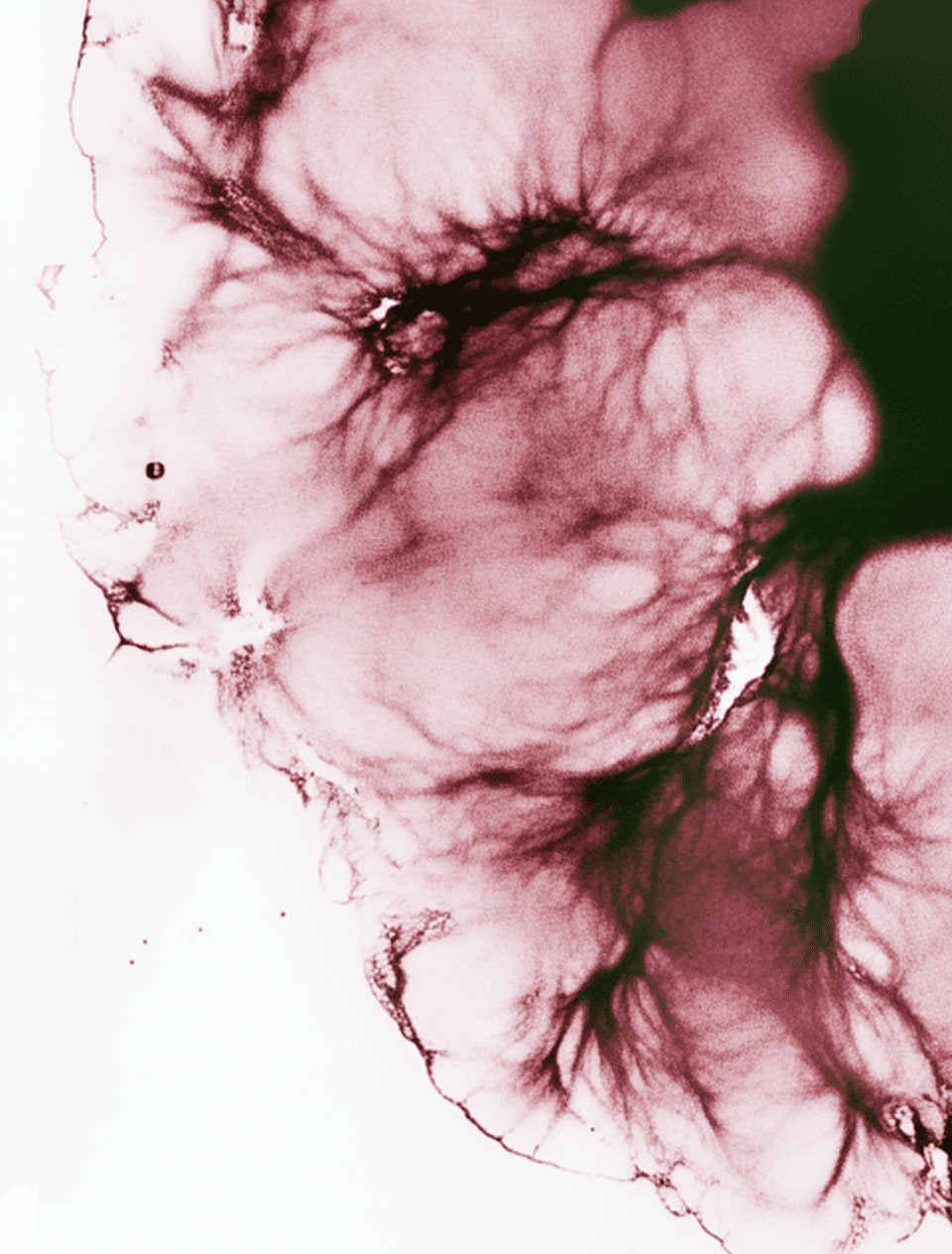
Our immunity relies on a complex network of specialized cells (macrophages, lymphocytes, dendritic cells, etc.) that work together to identify and eliminate pathogens. A key organ in this process is the thymus, which produces T lymphocytes. As we age, the thymus gradually shrinks (a phenomenon known as thymic involution or thymosenescence) which weakens the production of effective immune cells¹ ⁸.
Recent research has shown that, in animals, it is possible to reactivate the thymus using certain molecules like RANKL, with positive effects on immune response and lymphocyte production¹.
Nutrition, Vitamins, and Lifestyle: The Essential Foundations
Nutrition plays a crucial role in the normal functioning of the immune system. A varied diet rich in micronutrients helps meet the needs for vitamins and minerals involved in immune response⁷ ¹¹.
- Vitamin D: It helps regulate immune and inflammatory responses. Deficiency is common, especially in winter. ANSES recommends a monitored and individualized intake through food, sun exposure, or sensible supplementation¹¹.
- Zinc, iron, vitamins A, B9, B12, C, and E: These support the formation and activation of immune cells⁷.
- Moderate physical activity: It stimulates circulation and enhances immune vigilance, particularly by reducing the risk of acute respiratory infections⁶.
Dietary Supplements: Helpful or Risky?
Some dietary supplements, particularly herbal ones, are marketed to support immunity. However, ANSES warns that improper or prolonged use may disrupt the immune response¹⁰.
Certain herbs (echinacea, turmeric, cat’s claw...) act as anti-inflammatories and, in some cases, may hinder the necessary immune response during an infection¹⁰. It's therefore advised not to take them without medical advice, especially during illness or if you are immunocompromised.
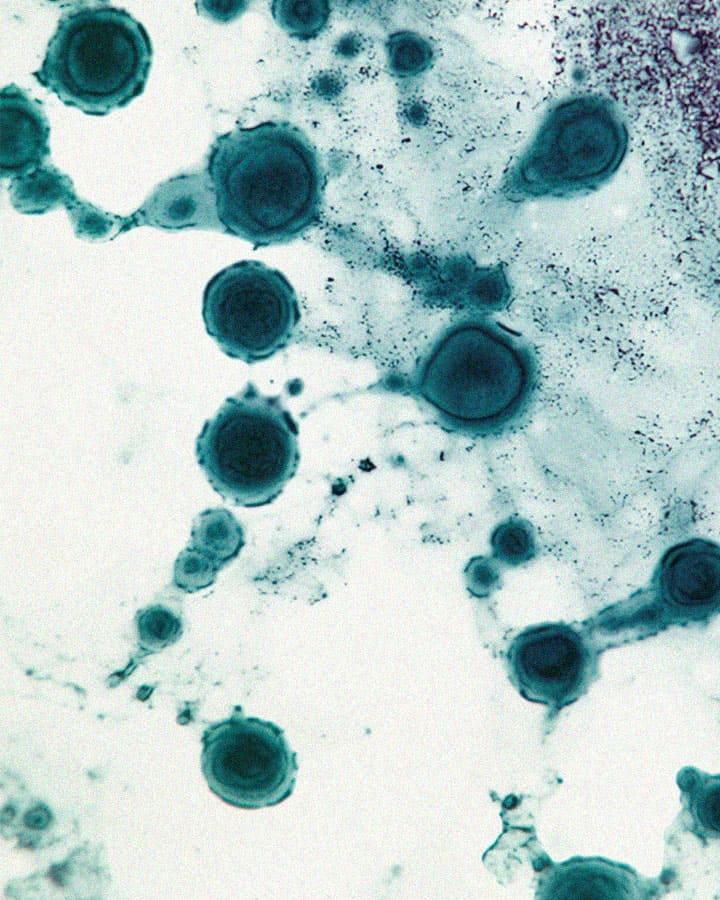
Weakened Immunity: Better Understanding Immune Deficiencies
Immune deficiencies can be:
- Primary, of genetic origin (e.g., severe combined immunodeficiency)⁴;
- Secondary, related to age, chronic diseases (diabetes, HIV, cancer), or treatments (chemotherapy, immunosuppressants)⁴.
They often result in repeated infections, reduced vaccine response, or increased susceptibility to certain diseases. Management involves accurate diagnosis, specialized medical follow-up, and sometimes treatments such as immunoglobulin therapy or stem cell transplantation⁴.
When Immunity Becomes Unbalanced: Autoimmune Diseases
Some conditions arise from a malfunctioning immune system that starts attacking the body’s own cells. These are known as autoimmune diseases (rheumatoid arthritis, lupus, type 1 diabetes, multiple sclerosis, etc.)⁵.
They affect around 8% of the population (mostly women) and have multifactorial origins: genetic, hormonal, and environmental⁵.
There is no cure, but targeted therapies can modulate immune responses and reduce symptoms⁵
Vaccination: A Recognized Pillar of Immune Protection
As the WHO highlights, vaccines simulate an infection in a controlled way to teach the immune system to recognize a pathogen without causing disease¹².
They promote the production of antibodies and memory lymphocytes, which can respond quickly to actual infections. Various types of vaccines exist (live-attenuated, inactivated, mRNA, etc.), each suited to a particular profile or context¹².
Vaccination remains one of the most effective means of preventing both individual and collective infectious diseases.
Looking Ahead: What Research Teaches Us
Immunology research is advancing rapidly. Institutions like Institut Curie, Inserm, CNRS, and others are exploring new mechanisms:
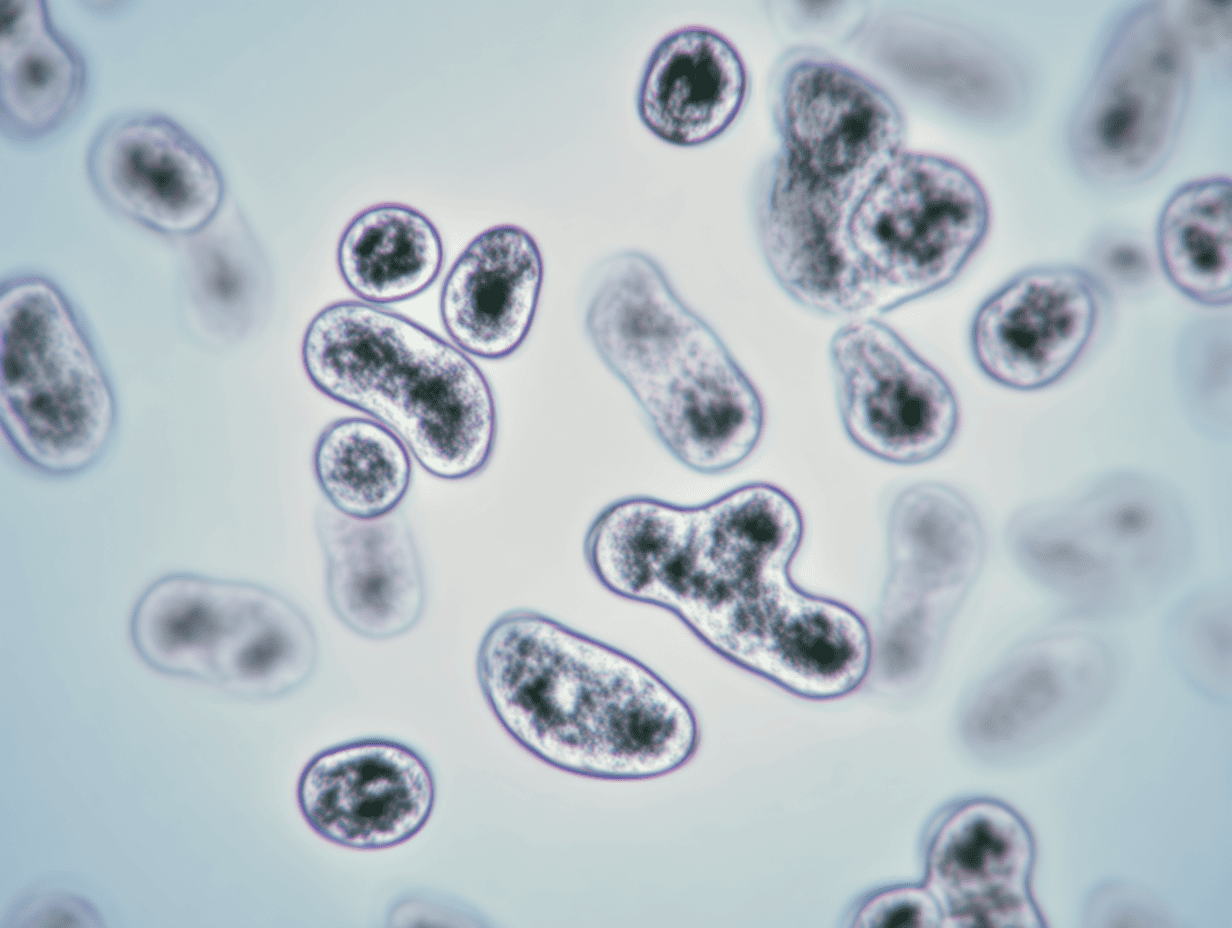
- Macrophages can extract energy from the bacteria they digest, boosting their efficiency even under nutritional stress² ³.
- Emerging approaches target cellular metabolism, autophagy, or the mTOR pathway, aiming to rebalance immunity, particularly in older adults⁸ ⁹.
These studies suggest promising personalized strategies to strengthen natural defenses in a targeted way.